Publish Date: 4 October 2025
Hip Impingement, or femoroacetabular impingement (FAI), is a condition where abnormal contact between the hip joint’s bones causes pain and restricts movement. Often affecting active individuals, it can lead to early osteoarthritis if untreated. Recognizing hip impingement symptoms, causes, and treatments is vital for restoring mobility. From hip impingement exercises to surgical options like hip arthroscopy, effective management can ensure a pain-free, active life. Early diagnosis via hip impingement xray or physical therapy is key. This syndrome, defined by a triad of symptoms, signs, and imaging findings, emphasizes the importance of comprehensive care to prevent long-term joint degeneration.
What Is Hip Impingement?
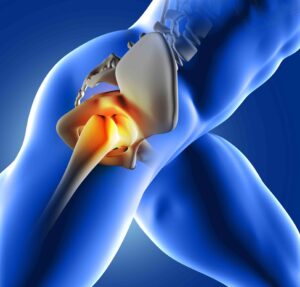
Hip impingement, also known as hip impingement syndrome or femoroacetabular impingement (FAI), is a mechanical disorder where the femoral head (ball) and acetabulum (socket) of the hip joint abnormally contact, damaging soft tissues like the labrum and cartilage. This leads to pain, reduced motion, and potential long-term complications. FAI is categorized into three main types: cam impingement, characterized by an aspherical femoral head that reduces the normal offset at the head-neck junction; pincer impingement, involving overcoverage of the acetabulum that pinches the labrum; or mixed impingement, which combines features of both cam and pincer morphologies, making it the most prevalent form [1, 2, 4]. These morphological variations disrupt the smooth gliding of the joint, leading to repetitive microtrauma over time [6, 8].
The condition is increasingly recognized as a significant contributor to hip pain in younger populations, particularly those without overt signs of arthritis on initial presentation [5, 9]. It involves subtle anatomical alterations that interfere with normal hip biomechanics, potentially accelerating the degenerative process toward osteoarthritis [4, 5, 6]. The acetabular labrum, a fibrocartilaginous ring that enhances joint stability by deepening the socket and providing a seal for synovial fluid, is frequently compromised in FAI, exacerbating instability and contributing to symptomatic progression [4, 10]. According to the 2016 Warwick Agreement consensus, FAI is defined by a diagnostic triad encompassing symptoms, clinical signs, and radiographic findings, which helps differentiate it from other hip pathologies such as bursitis or muscle strains [1, 3].
In cam-type FAI, the femoral head-neck junction lacks the typical concave offset, causing it to impinge against the acetabular rim during activities involving hip flexion, much like a cam mechanism in machinery [6, 7]. Pincer-type FAI arises from excessive acetabular coverage, often due to retroversion or protrusion, which traps the labrum between the bones during motion [6, 7]. Mixed FAI, being the most common, integrates elements of both, resulting in compounded repetitive trauma and progressive joint damage [8]. This abnormal mechanical process is not just a static deformity but a dynamic issue exacerbated by vigorous hip movements, highlighting why it often manifests in athletes or active individuals [1, 6].
Understanding hip impingement is essential because it can mimic other conditions like groin strains, hernias, or even lower back issues, often leading to delayed diagnosis and prolonged suffering [9]. Early recognition through a thorough patient history, physical examination, and appropriate imaging can prevent irreversible damage, underscoring the importance of awareness among athletes, active individuals, and healthcare providers. Moreover, as FAI is implicated in the pathophysiology of early-onset osteoarthritis, addressing it promptly may alter the disease trajectory and preserve joint function for years to come [5, 6, 8].
What Causes Hip Impingement?
Hip impingement is primarily driven by morphological abnormalities in the hip joint’s bony structures, which create premature contact during movement. Cam deformities involve an aspherical femoral head that bulges at the head-neck junction, leading to abnormal contact especially during hip flexion and internal rotation [2, 6, 10]. Pincer deformities, on the other hand, stem from excessive acetabular coverage, such as global overcoverage or focal retroversion, which compresses the labrum against the femoral neck [2, 6]. A combination of both, known as mixed impingement, is frequently observed and amplifies the mechanical stress on the joint [2, 8].
Genetic factors play a substantial role, with familial patterns of FAI morphology observed, suggesting hereditary predispositions to these bony alterations [2]. Environmental influences further contribute, particularly repetitive high-impact activities during adolescence, such as those in sports requiring maximal hip flexion like soccer, hockey, or ice skating, which can promote the development of cam morphology by stimulating abnormal bone growth at the physeal plate [1, 4]. The etiology encompasses a pathologic mechanical process where these bony anomalies, combined with vigorous hip motion, result in repetitive collisions that progressively damage soft tissues including the labrum, cartilage, and surrounding structures [6, 8, 10].
Less is understood about the precise development of pincer morphology, but it may involve acetabular overgrowth, protrusio acetabuli, or retroversion, potentially influenced by both genetic and mechanical factors during skeletal maturation [1, 4]. Structural abnormalities at the femoral head-neck junction or acetabulum cause abnormal abutment during terminal hip motion, often remaining asymptomatic or undiagnosed for years until cumulative damage manifests as pain [9]. In some instances, altered bony morphology of the proximal femur and acetabulum not only impairs function but also predisposes to early osteoarthritis by initiating a cascade of joint degeneration [5, 8].
Repetitive trauma from impingement generates progressive wear at the acetabular labrum, chondrolabral junction, and articular cartilage, creating a vicious cycle of inflammation and further structural compromise [8, 10]. Premature contact during everyday or athletic hip motions, driven by aspherical femoral deformities or acetabular overcoverage, exacerbates this issue, highlighting the interplay between anatomy and activity [6, 10]. Overall, FAI represents a multifactorial condition where innate skeletal variations interact with lifestyle factors to produce symptomatic impingement.
Hip Impingement Risk Factors
Risk factors for hip impingement encompass demographic, genetic, and lifestyle elements that heighten susceptibility. Younger age groups, particularly adolescents and young adults, are at increased risk due to the developmental window during which bony morphologies form [2, 4]. Caucasian background is associated with higher prevalence, possibly linked to genetic predispositions [2]. Participation in high-intensity sports during adolescence, such as those involving repetitive hip loading and extreme ranges of motion, significantly promotes cam deformity development by inducing adaptive bone changes [1, 2, 4].
Familial FAI morphology further increases risk, indicating a strong genetic component where inherited skeletal traits predispose individuals to impingement [2]. Athletes in disciplines like soccer, hockey, ballet, or martial arts face elevated risks owing to the repetitive hip flexion and rotation demands that stress the joint [1, 4]. Gender differences are notable: males are more prone to cam-type FAI due to higher rates of physeal stress, while females may lean toward pincer-type, though mixed forms dominate across both [4]. Previous hip injuries, such as labral strains or fractures, or developmental conditions like slipped capital femoral epiphysis (SCFE) or Legg-Calvé-Perthes disease, can alter joint anatomy and predispose to FAI [4, 9].
Additionally, obesity may exacerbate symptoms by increasing joint load, though it’s not a primary cause; conversely, highly active lifestyles during growth periods are more directly tied to morphological changes [4]. Occupational factors involving prolonged sitting or repetitive twisting motions can also contribute to symptom onset in predisposed individuals. Understanding these risk factors allows for targeted prevention strategies, such as modified training regimens for young athletes.
What Are Hip Impingement Symptoms?
Hip impingement symptoms often emerge gradually, with slow-onset, persistent groin pain being the most common initial complaint, affecting daily activities and sports performance [2, 3, 5]. Patients frequently report discomfort exacerbated by hip flexion, adduction, and internal rotation maneuvers, which can be elicited through a positive FADIR (flexion, adduction, internal rotation) test, also termed the impingement sign [2, 10]. Additional manifestations include mechanical symptoms such as clicking, catching, locking, buckling, stiffness, or a sensation of giving way, reflecting underlying labral or cartilage involvement [8, 10].
Bilateral hip pain is not uncommon, particularly in cases where morphological abnormalities affect both sides, leading to symmetrical symptoms that develop over years [9]. Pain may radiate to adjacent areas like the lower back, buttocks, or thigh, often mimicking other pathologies such as lumbar radiculopathy or trochanteric bursitis, which complicates diagnosis [7, 9]. Activities that provoke symptoms typically involve deep hip flexion, such as squatting, pivoting, climbing stairs, or prolonged sitting in low chairs, which can significantly impact quality of life, work, and recreational pursuits [7, 10].
In advanced stages, patients might experience night pain or rest pain, indicating progressive joint damage [5]. The pain is often described as deep and aching, sometimes with sharp exacerbations during specific movements, and may be accompanied by reduced range of motion, particularly in internal rotation [2, 10]. These symptoms underscore the importance of early intervention to halt progression.
What Are the Complications of Hip Impingement?
Untreated hip impingement poses significant risks, primarily through progressive damage to the labrum, articular cartilage, and other joint structures, which predisposes individuals to early-onset osteoarthritis (OA) [2, 4, 5, 6]. Repetitive impingement forces generate chondral lesions, delamination of cartilage, and labral pathology, accelerating degenerative changes within the hip joint [6, 7, 8, 10]. This mechanical wear creates a pathway for OA development, where initial subtle abnormalities evolve into irreversible joint destruction [5, 8].
Long-term complications may necessitate advanced interventions like total hip arthroplasty, especially in cases with prominent cam deformities that elevate OA risk in middle-aged adults [6]. Chronic pain, persistent stiffness, and diminished mobility can lead to decreased quality of life, functional limitations, and psychological impacts such as depression or anxiety related to activity restrictions [5]. Secondary complications include muscle imbalances from compensatory gait patterns, potentially causing issues in the lower back, knees, or contralateral hip [4]. In athletes, untreated FAI may result in career-ending injuries or permanent performance deficits [1]. Overall, the progressive nature of FAI highlights the need for timely management to mitigate these outcomes.
How Is Hip Impingement Diagnosed?
Diagnosis of hip impingement requires a multifaceted approach, beginning with a comprehensive patient history that explores the onset, location, and aggravating factors of groin pain, often activity-related [7, 8, 10]. Physical examination is pivotal, incorporating provocative maneuvers such as the FADIR test (flexion, adduction, internal rotation) to reproduce impingement symptoms, and the FABER test (flexion, abduction, external rotation) to assess flexibility and pain [8, 10]. These tests help identify positive impingement signs indicative of FAI [2, 10].
The diagnostic triad of FAI syndrome—symptoms, clinical signs, and imaging abnormalities—must be confirmed to establish the condition [3]. Early detection is crucial, as symptoms can persist undiagnosed for extended periods, allowing damage to accumulate [9]. Clinicians should differentiate FAI from other causes of hip pain, such as avascular necrosis or stress fractures, through systematic evaluation [7].
What Tests Will Be Done to Diagnose Hip Impingement?
Diagnostic testing for hip impingement commences with plain radiographs, including anteroposterior (AP) pelvis views, to evaluate bony morphology [2, 7, 8]. Key measurements include the alpha angle for cam deformities (typically >50-55 degrees indicating abnormality) and the lateral center-edge angle for pincer deformities ( >40 degrees suggesting overcoverage) [2, 7]. Specialized views like the Dunn 45-degree lateral or false-profile projection aid in identifying classic signs such as the pistol-grip deformity in cam FAI or the crossover sign in pincer FAI [7].
Advanced imaging modalities enhance detection of soft tissue involvement. Magnetic resonance imaging (MRI) or magnetic resonance arthrography (MRA) is superior for visualizing labral tears, cartilage defects, and intra-articular pathology, with MRA providing better contrast for subtle lesions [7, 8, 10]. Computed tomography (CT) scans offer detailed three-dimensional assessment of bony architecture, useful for surgical planning [7]. These tests are essential for confirming cam or pincer morphology, as pathological thresholds remain somewhat variable [3]. In complex cases, diagnostic intra-articular injections can help localize pain sources [1].
How Is Hip Impingement Treated?
Treatment for hip impingement focuses on alleviating pain, enhancing function, and halting progression to osteoarthritis, with strategies tailored to symptom severity and patient goals [1, 3, 5]. Initial management often involves conservative measures, transitioning to surgery if symptoms persist [1, 3].
Non-Surgical Treatment Options
Non-surgical interventions serve as the first-line approach for mild to moderate cases, emphasizing activity modification to avoid provocative positions, non-steroidal anti-inflammatory drugs (NSAIDs) for pain control, and physiotherapist-led therapy to optimize hip and pelvic kinematics [3, 8, 10]. Therapeutic exercises target muscle imbalances, improve proprioception, and reduce impingement during motion [10]. Intra-articular corticosteroid or hyaluronic acid injections may provide temporary symptomatic relief, although supporting evidence is limited and they are not curative [1]. These methods can significantly improve quality of life without invasive risks, particularly in patients with minimal structural damage [3].
Surgical Treatment (Hip Arthroscopy)
For refractory cases, hip impingement surgery, predominantly hip arthroscopy, is the gold standard, addressing bony deformities and associated soft tissue injuries [1, 2, 3, 7, 8, 10]. The procedure entails femoral osteochondroplasty to reshape the cam lesion, acetabular rim trimming for pincer overcoverage, and labral repair or debridement to restore joint integrity [7]. Arthroscopic techniques offer minimally invasive benefits, including shorter recovery times and lower complication rates compared to open surgery, with equivalent outcomes [7]. However, risks such as infection, nerve injury, or incomplete correction exist, and not all patients return to pre-injury activity levels [1]. Surgery is particularly effective in younger patients without advanced OA [1, 6].
Rehabilitation and Physical Therapy Tips
Rehabilitation is integral to both non-surgical and post-surgical management, focusing on phased programs that incorporate postural control, core stabilization, hip strengthening, motor control, and mobility enhancement [10]. Hip impingement exercises may include pelvic tilts for alignment, bird dog for core engagement, clam shells for gluteal activation, bridges for posterior chain strength, and dynamic stretches like pigeon pose or banded hip distractions to improve flexibility [10]. Postoperatively, protocols emphasize protected weight-bearing initially, progressing to functional training over 3-6 months [1, 3, 10]. Patient education on proper biomechanics and gradual return to activity is essential to prevent recurrence and optimize long-term outcomes [10].
Hip Impingement Treatment in Turkey
Turkey has emerged as a prominent destination for hip impingement treatment, leveraging advanced medical infrastructure and experienced orthopedic specialists to offer comprehensive care at competitive costs. Facilities in major cities like Samsun and Antalya provide state-of-the-art diagnostic tools, including high-resolution MRI and CT imaging, to accurately assess FAI morphology [1, 3]. Non-surgical options, such as customized hip impingement physical therapy programs, are widely available, focusing on evidence-based exercises to manage symptoms conservatively [10]. For surgical candidates, hip arthroscopy is performed using cutting-edge minimally invasive techniques, with surgeons skilled in addressing cam, pincer, and mixed impingements while preserving joint function [1, 7].
Turkish clinics often integrate multidisciplinary teams, including physiotherapists and sports medicine experts, to deliver personalized rehabilitation plans that align with international standards [3, 10]. The emphasis on early intervention helps mitigate progression to osteoarthritis, and many centers offer packages that include pre-operative assessments, surgery, and post-operative care [1]. Medical tourism in Turkey combines high-quality treatment with affordability, attracting international patients seeking effective solutions for hip impingement syndrome.
What Is the Recovery Time for Hip Impingement?
Recovery timelines for hip impingement vary based on treatment modality, patient factors, and adherence to rehabilitation. For non-surgical management, such as physical therapy and activity modification, noticeable improvements in pain and function can occur within 6-12 weeks, though full symptom resolution may take 3-6 months with consistent effort [3, 10]. Patients are encouraged to monitor progress and adjust activities to prevent flare-ups [10].
Following hip arthroscopy, initial recovery involves 4-6 weeks of limited weight-bearing and protective measures to allow tissue healing, with light activities resuming thereafter [1, 2]. Full functional recovery typically spans 3-6 months, incorporating progressive physical therapy to rebuild strength and mobility [1, 3]. Athletes or highly active individuals may require 6-12 months to return to competitive levels, with outcomes influenced by pre-surgical OA presence and no assurance of complete restoration [1]. Short-term results favor surgery over conservative care for symptom relief, but long-term impacts on OA prevention remain under investigation [3]. Regular follow-up ensures optimal recovery.
Can I Prevent Hip Impingement?
Preventing hip impingement centers on mitigating modifiable risk factors, particularly during critical growth periods in adolescence. Avoiding or moderating excessive participation in high-impact sports that demand repetitive hip flexion and rotation can reduce the likelihood of developing cam deformities [1, 2, 4]. Incorporating balanced training programs that emphasize proper technique, warm-ups, and recovery can minimize joint stress [4, 10].
Maintaining optimal hip flexibility, strength, and core stability through targeted hip impingement exercises, such as yoga-inspired stretches or strength routines, supports joint health [10]. Early screening for at-risk populations, including young athletes or those with family history, via physical exams or imaging, enables proactive interventions [4]. While genetic predispositions cannot be altered, lifestyle modifications like weight management and ergonomic adjustments in daily activities can lessen symptom onset in susceptible individuals [2, 4]. Education on body mechanics and gradual activity progression is key to prevention strategies.
References
- Griffin DR, et al. Femoroacetabular Impingement Syndrome. Nat Rev Dis Primers. 2020;6(1):75. https://pubmed.ncbi.nlm.nih.gov/32925375/
- Leong N, et al. An Updated Review of Femoroacetabular Impingement Syndrome. Orthop Clin North Am. 2022;53(4):431-440. https://pubmed.ncbi.nlm.nih.gov/36034731/
- Peters S, et al. Femoroacetabular impingement – What the rheumatologist needs to know. Best Pract Res Clin Rheumatol. 2024;38(1):101925. https://pubmed.ncbi.nlm.nih.gov/38336510/
- McClincy MP, et al. Femoroacetabular Impingement and Acetabular Labral Tears – Part 1. Orthop J Sports Med. 2020;8(10):2325967120954342. https://pubmed.ncbi.nlm.nih.gov/33093713/
- Ganz R, et al. Femoroacetabular impingement: a common cause of hip pain. Phys Sportsmed. 2018;46(2):139-144. https://pubmed.ncbi.nlm.nih.gov/29406812/
- Leunig M, et al. Femoroacetabular impingement: defining the condition and its role in the pathophysiology of osteoarthritis. J Am Acad Orthop Surg. 2013;21 Suppl 1:S2-S8. https://pubmed.ncbi.nlm.nih.gov/23818194/
- Bedi A, et al. Femoroacetabular impingement: a review of diagnosis and management. Curr Rev Musculoskelet Med. 2011;4(1):23-32. https://pubmed.ncbi.nlm.nih.gov/21475562/
- Martinez JR, et al. Review of femoroacetabular impingement syndrome. Orthop Clin North Am. 2024;55(4):447-458. https://pubmed.ncbi.nlm.nih.gov/39839560/
- Ganz R, et al. Femoroacetabular impingement: an overlooked cause of hip pain. Am J Orthop (Belle Mead NJ). 2006;35(6):267-271. https://pubmed.ncbi.nlm.nih.gov/16715026/
- Voight ML, et al. Therapeutic Exercise Approaches to Nonoperative and Postoperative Management of Femoroacetabular Impingement Syndrome. J Athl Train. 2020;55(11):1155-1164. https://pubmed.ncbi.nlm.nih.gov/33112956/

Assoc. Prof. Dr. Ömer Bozduman completed his medical degree in 2008 and subsequently served in various emergency medical units before finishing his Orthopedics and Traumatology residency in 2016. After working at Afyonkarahisar State Hospital, Tokat Gaziosmanpaşa University, and Samsun University, he continued his career at Memorial Antalya Hospital. He now provides medical services at his private clinic in Samsun, specializing in spine surgery, arthroplasty, arthroscopy, and orthopedic trauma.



